Alcohol Withdrawal
Articles:
1. This is not a protocol designed for intubated patients because it relies on CIWA to determine when someone is moving from no ETOH withdrawal to uncomplicated ETOH withdrawal to complicated ETOH withdrawal and CIWA is not a good scoring system for an intubated patient who can’t answer questions. Regardless, we are extrapolating it to intubated patients which isn't necessarily wrong.
2. Clonidine and precedex both act as alpha-2 adrenergic receptor agonist which is why they can both cause bradycardia. I did a pubmed search and didn’t find any studies which looked at combining the two agents together for ETOH withdrawal. So adding clonidine to precedex may not be beneficial, but adding clonidine if you are weaning precedex may be
3. The dose of clonidine in the study for prophylaxis is clonidine 0.1 mg TD + clonidine 0.1 mg po/IV q8h x 3 doses. I currently can’t pull up EPIC to check the order set but I don’t remember doing the bolus dose that they were doing. It would be appropriate given the slow action of the TD
4. Guanfacine is a more selective alpha agent than clonidine and causes less sedation and hypotension. I can’t check our formulary right now. But consider this as an alternative to clonidine in some patients. This can also be used to transition patients off long term precedex (Mrs Smith and her anxiety comes to mind) . This is not a medication I'm familiar with.
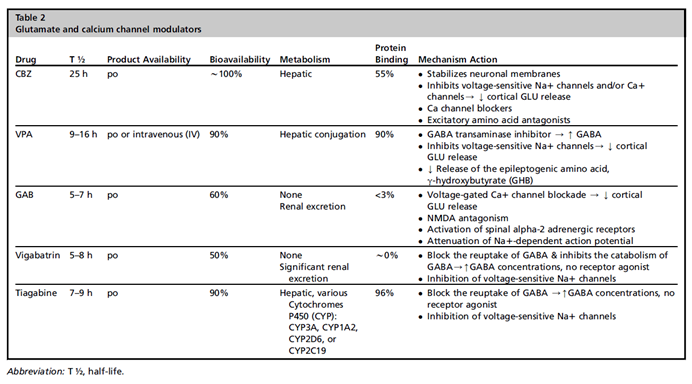
5. In renal failure avoid gabapentin because it is renally metabolized. They choose gabapentin to include in the study because they worry about cirrhosis in ETOH withdrawal patients. I actually would argue that more of our ETOH withdrawal patients in the ICU have renal injury than cirrhosis. They are drinkers that show up in the ICU for other reasons (sepsis, MVA) rather than decompensated cirrhosis or primary withdrawal. The alternative agents to gabapentin are carbamazepine and valproic acid. Both undergo hepatic instead of renal metabolism. Carbamazepine actually looks like it has pretty good evidence behind it and it has a nice long half-life which I prefer in prophylaxis and treatment of withdrawal. It is po only and I’m not sure if it can go down a tube. VPA is po or IV.
6. They have electrolyte goals, in particular a magnesium goal of 1.7 to 2.2. They also show magnesium in figure 1 as acting directly on the NMDA channel. Magnesium is also a treatment for some seizures. I started looking to see if there is any good literature on using magnesium to treat ETOH withdrawal. There isn’t. There is a Cochrane review from 2012 (https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008358.pub2/full) that goes through four studies but none of the studies are well designed and only one uses IV mag. So, although this piques my interest, there is no data. But, the next time I see an alcohol withdrawal seizure I will try to remember to also give 4-6 grams of IV magnesium as well as all the normal interventions. This brings up a great point that I heard recently in an anesthesia podcast I’ve been listening to (can’t remember which episode or I’d include a link). The guest speaker was talking about how in non-OB fields we shy away from higher doses of magnesium even when they are indicated. He talked about the 2 grams IV mag we always give and then compared it to OB. In OB for eclampsia and seizures they treat with much higher doses (4-6g load over 20-30 minutes, followed by 1-2g/hr continuous infusion) and have few side effects (there are some you have to watch for though). You wouldn't want to give those kind of doses to someone in renal failure. But if the kidneys are working and someone was having an ETOH seizure a 4-6 gram load over 20 minutes would not be inappropriate, though you may have to convince nursing that it was safe. The reason you may need higher doses is because the plasma levels of Mag don't necessarily correlate to CSF levels (per this article).